The sodium/glucose cotransporter 2 inhibitor empagliflozin is a pharmacological chaperone of cardiac Nav1.5 channels
The sodium/glucose cotransporter 2 inhibitor empagliflozin is a pharmacological chaperone of cardiac Nav1.5 channels
Sauer, J.; Marksteiner, J.; Hohenegger, M.; Todt, H.; Kubista, H.; Dostal, C.; Kiss, A.; Podesser, B. K.; Salzer, I.; Koenig, X.; Stary-Weinzinger, A.; Hilber, K.; Kudlacek, O.
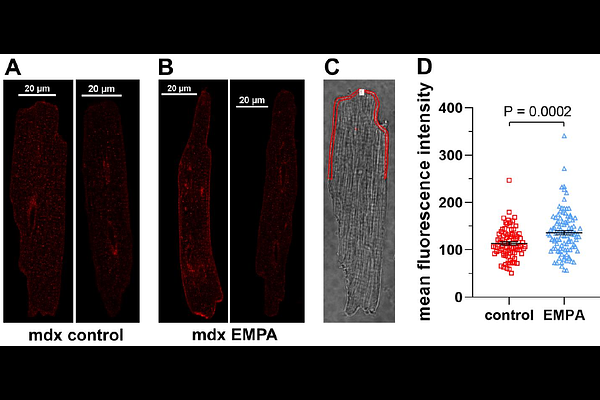
AbstractDiminished peak sodium current (INa) is a causative factor for slowed ventricular conduction and cardiac arrhythmias in patients with Duchenne muscular dystrophy (DMD), a devastating muscle disease triggered by dystrophin deficiency. Recently, we showed that chronic administration of the sodium/glucose cotransporter 2 (SGLT2) inhibitor empagliflozin (EMPA) restores diminished peak INa in ventricular cardiomyocytes from the dystrophin-deficient mdx mouse model of DMD. Here, we aimed to elucidate the underlying mechanism. Whole cell patch clamp studies revealed that 24 h incubation of dystrophic (mdx) ventricular cardiomyocytes with EMPA significantly increases peak INa in a concentration-dependent manner (EC50=94 nM). The enhancing effect on peak INa also occurred in dystrophic cardiac Purkinje fibers, Nav1.5-expressing tsA201 cells, as well as in dystrophic (DMDmdx) rat cardiomyocytes, and was also exerted by two other SGLT2 inhibitors. Immunofluorescence studies suggested that chronic EMPA treatment increases Nav1.5 plasma membrane expression. Peak INa enhancement by EMPA depended on functional anterograde trafficking of Nav1.5. The local anesthetic mexiletine, a well-known pharmacological chaperone of Nav1.5, enhanced peak INa in a similar manner as EMPA. Further, mutation of human Nav1.5 at a site important for local anesthetic binding (Y1767A) completely abolished the ability of both EMPA and mexiletine to enhance peak INa. Finally, the importance of Y1767 for drug-induced modulation of peak INa was confirmed by molecular docking simulations. Our findings suggest that EMPA acts as a pharmacological chaperone of Nav1.5 channels. Its chronic administration may reduce arrhythmia vulnerability in patients with DMD and other arrhythmogenic pathologies associated with diminished peak INa.